
Choroid Plexus Carcinoma (CT post embolization)
Findings:
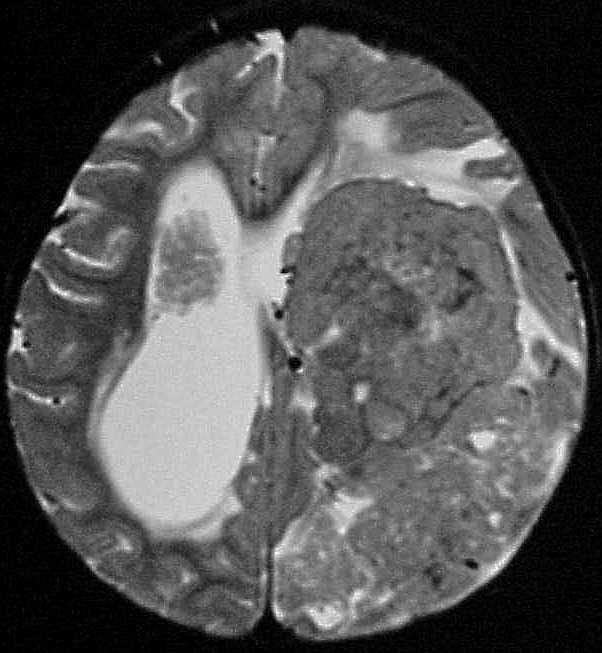
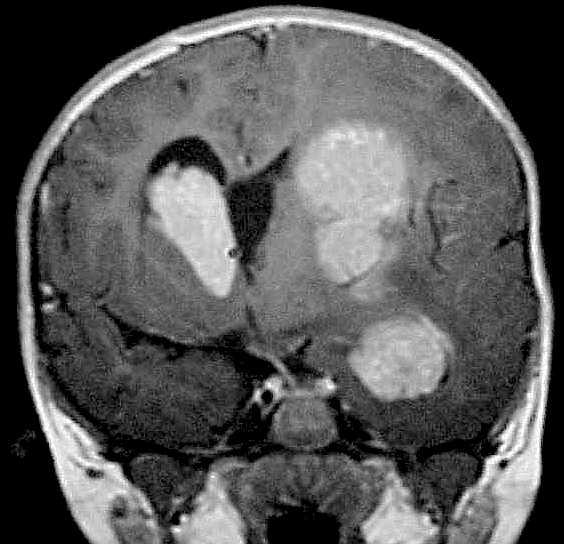
Multiple MR images show a large, multifocal, homogenously
enhancing intraventricular mass associated with hydrocephalus and left
to right midline shift. The masses exhibit heterogenous isointensity on
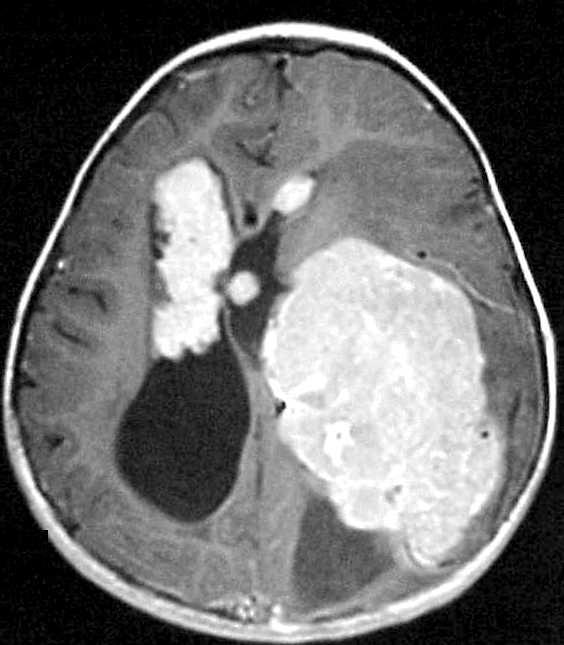
T2. The CT image obtained after preoperative embolization shows a large
amount of contrast stasis within the left cerebral hemisphere in the region
of previously noted tumor. The very low attenuation foci that look like
gas bubbles are actually PVA particles, some of which have a linear vascular
distribution in the parietal region. A metallic coil is also present.
Differential Diagnosis:
This represents a highly aggressive neoplasm, of which
choroid plexus carcinoma is the most likely diagnosis. Other tumors to
consider would include intraventricular GBM, PNET, or possibly meningioma.
Intraventricular meningioma is rare, but would be even more uncommon in
a child of this age.
Discussion:
Choroid plexus tumors are most common in the first decade
and represent approximately 0.5% of all intracranial neoplasms. However,
it is one of the most common brain tumors in patients less than 2 years
old. In children, the tumors arise most commonly in the trigone of the
lateral ventricle. In adults, a fourth ventricular origin is more common.
Hydrocephalus may be caused by overproduction of CSF and/or resorption
impairment due to hemorrhage, increased protein content, and tumor pieces.
CSF seeding is common. Malignant degeneration is found in 10-20%, and imaging
can't usually distinguish between benign and malignant. Imaging features
include iso/hyperdense on CT, iso T1, iso/hyper T2, and marked enhancement.
Calcification is seen in approximately 25%. Choroid plexus calcification
in a patient less than 10 should suggest the developmant of CP papilloma.
Preoperative embolization is occasionally helpful, with vascular supply
from anterior choroidal, lateral posterior choroidal, and medial posterior
choroidal arteries.