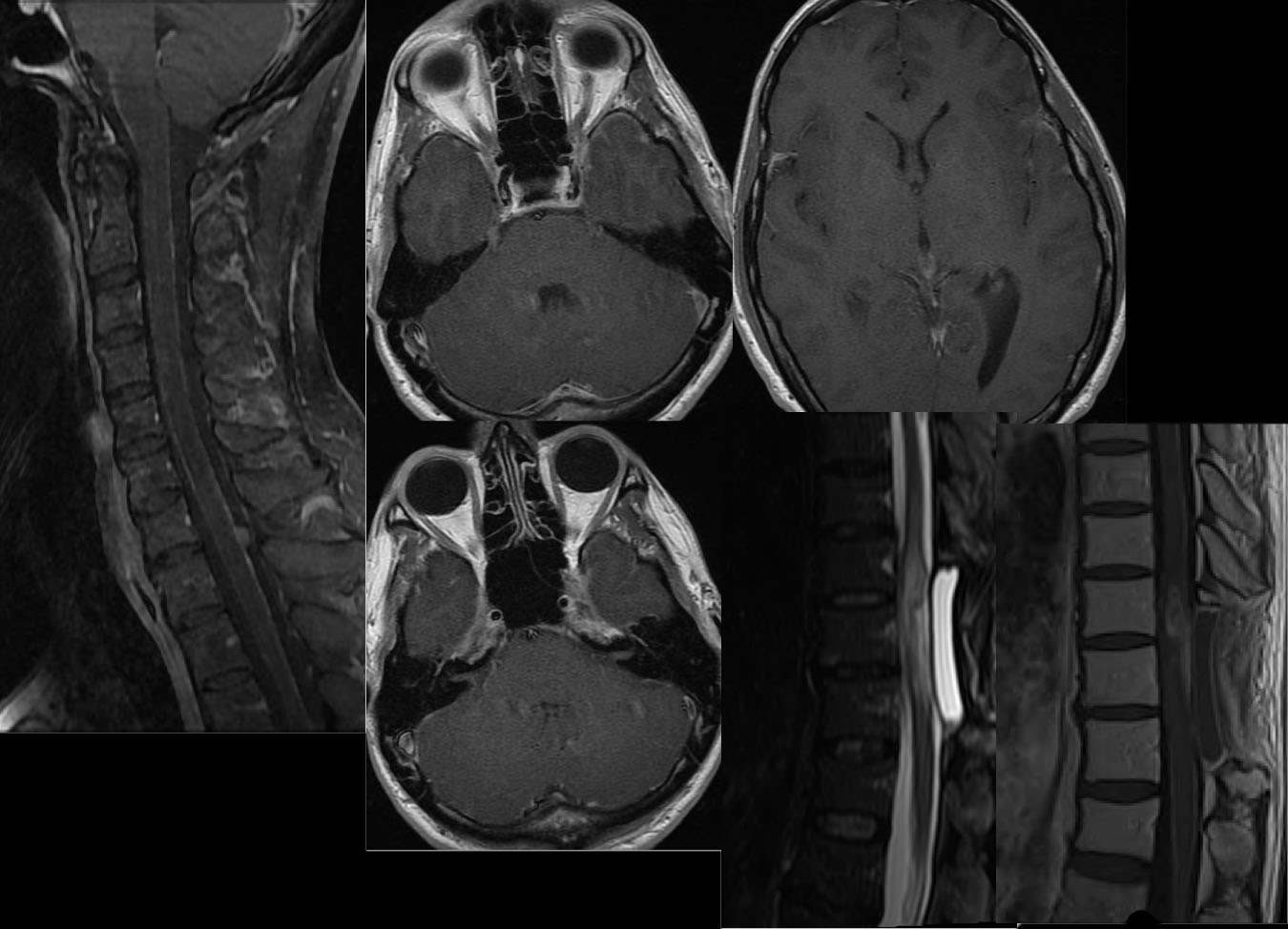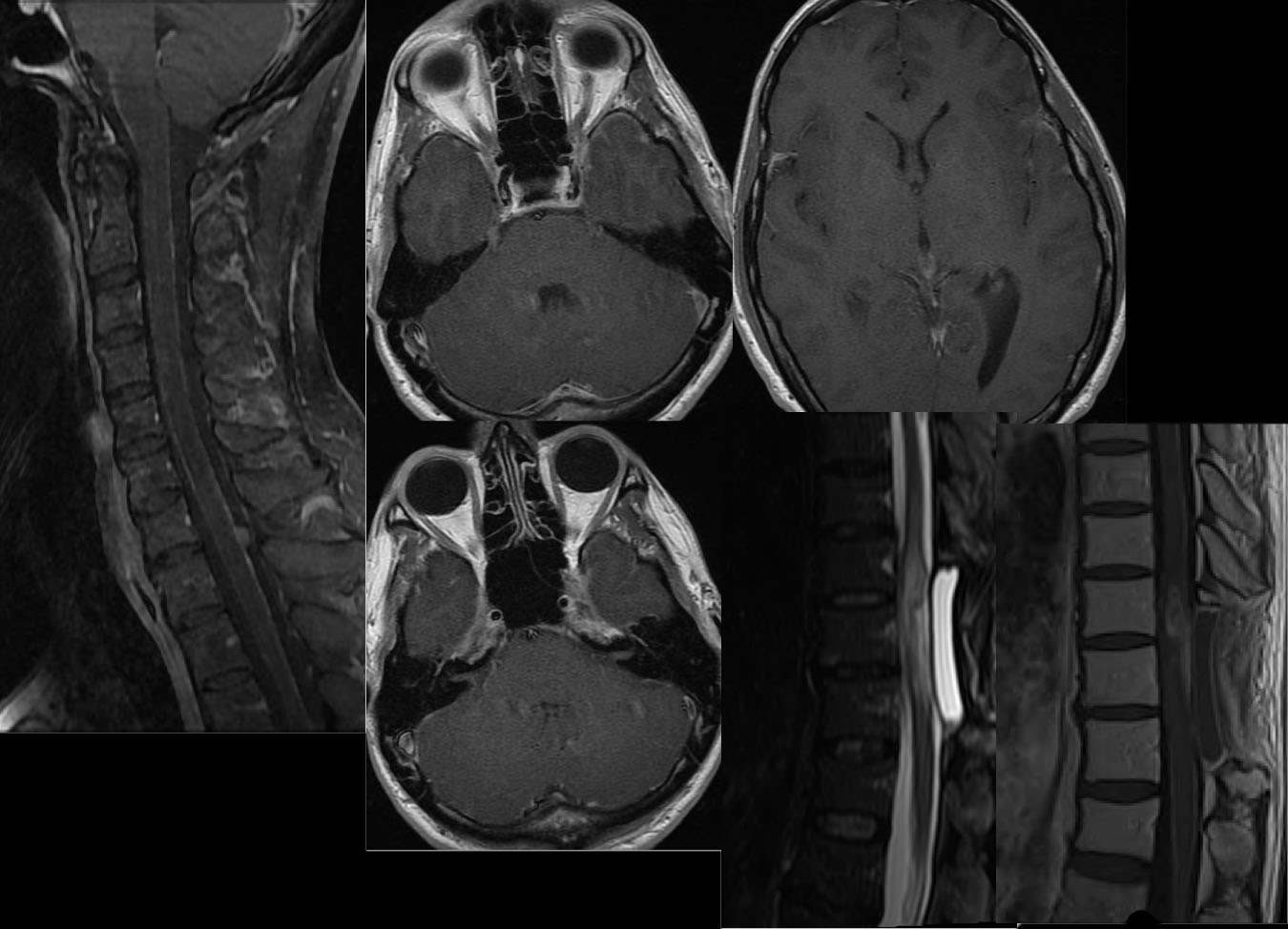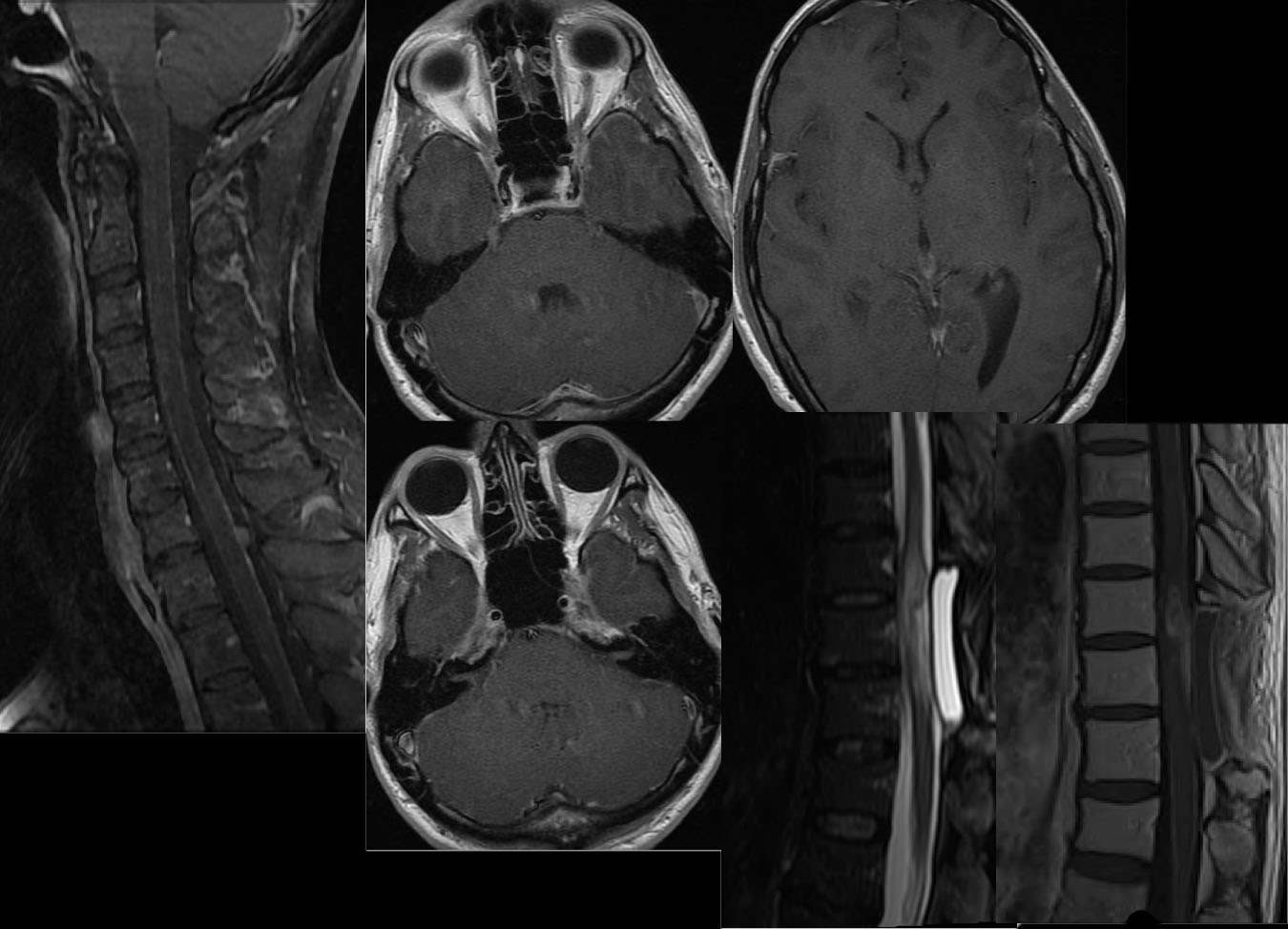
Spinal glioblastoma multiforme with recurrence and CSF tumor dissemination
Findings:
Multiple MR images demonstrate postoperative changes of thoracic laminectomy with underlying cord expansion and abnormal nodular intramedullary enhancement. Additional abnormal enhancement coats the spinal cord with focal nodule posteriorly at C7-T1. There is also abnormal subarachnoid enhancement coating cranial nerves V and VII/VIII, and additional subtle leptomeningeal enhancement along the temporal lobes and lateral sylvian fissures.
Differential diagnosis:
Tumor recurrence with CSF mets, infection less likely, normal enhancement of vessels along cord less likely. Sometimes need to compare some normals to realize this is abnormal, if you don't initially see the nodule at C7-T1.
Discussion:
GBM is the
most common intracranial glioma, with an age peak of 45-55, M>F. Spinal cord GBM is uncommon. Of high grade spinal cord neoplasms, most are WHO grade III anaplastic astro. Intramedullary malignant neoplasms essentially always enhance, and the typical differential is ependymoma and astrocytoma. Astro is more infiltrative in a younger age group and Ependymomass are more commonly hemorrhagic and assd with complex cysts/syrinx. Microscopically wide
invasion is the rule despite possibly having a well circumscribed appearance.
GBM may have occasional calcification and may be markedly hypervascular
with flow voids, simulating AVM on angio. The tumor may become more necrotic
and calcified with treatment. Prognosis is dismal, with a median survival
measured in months.
BACK TO
MAIN PAGE