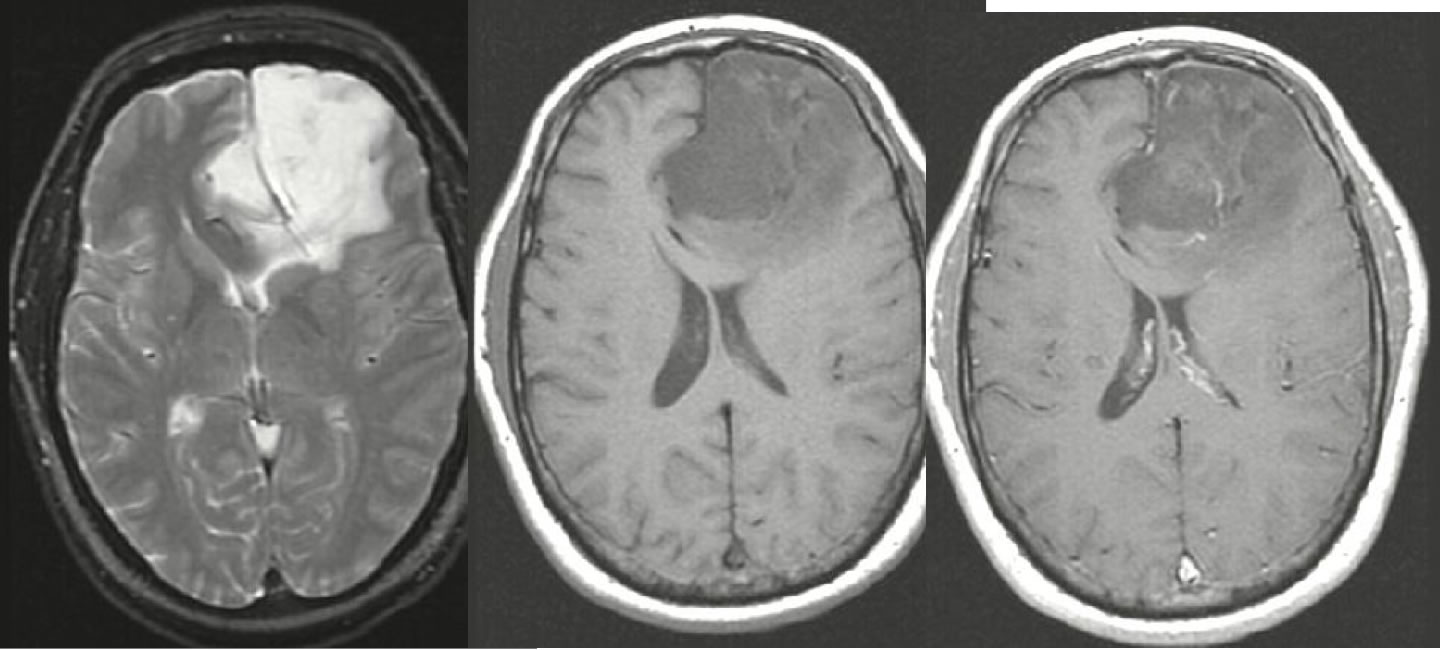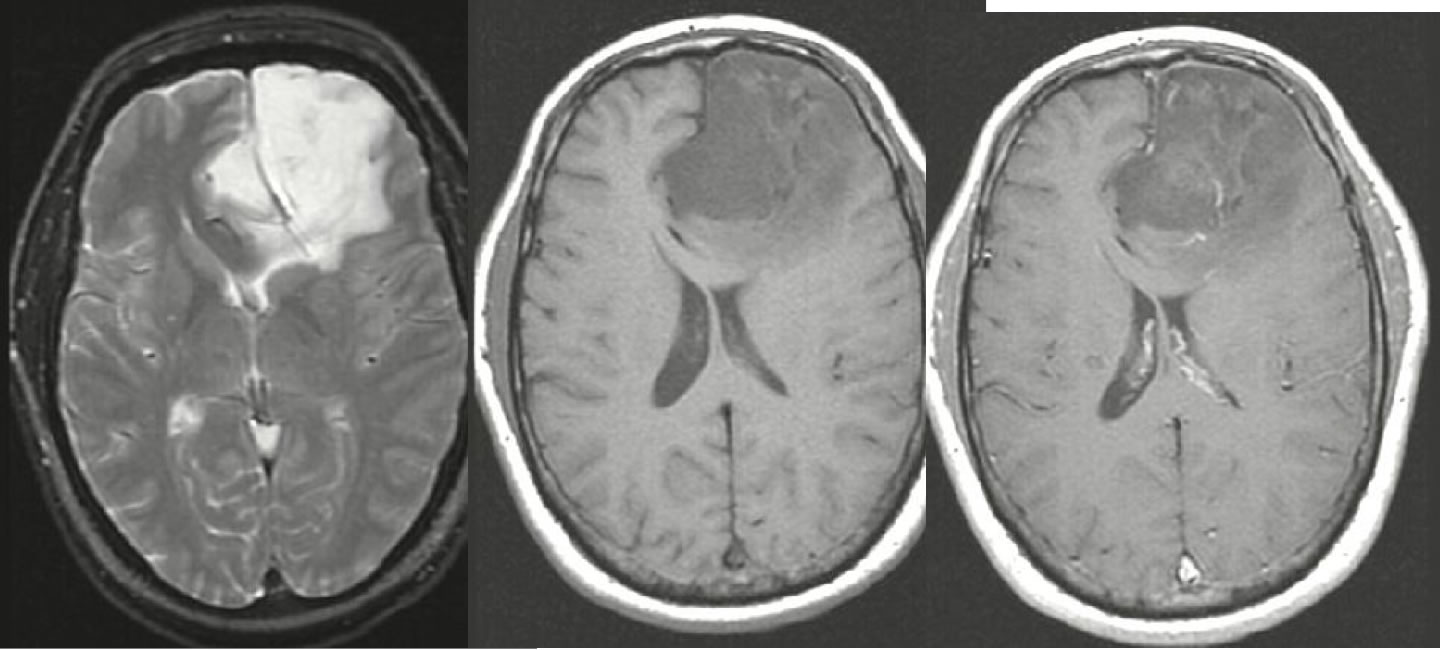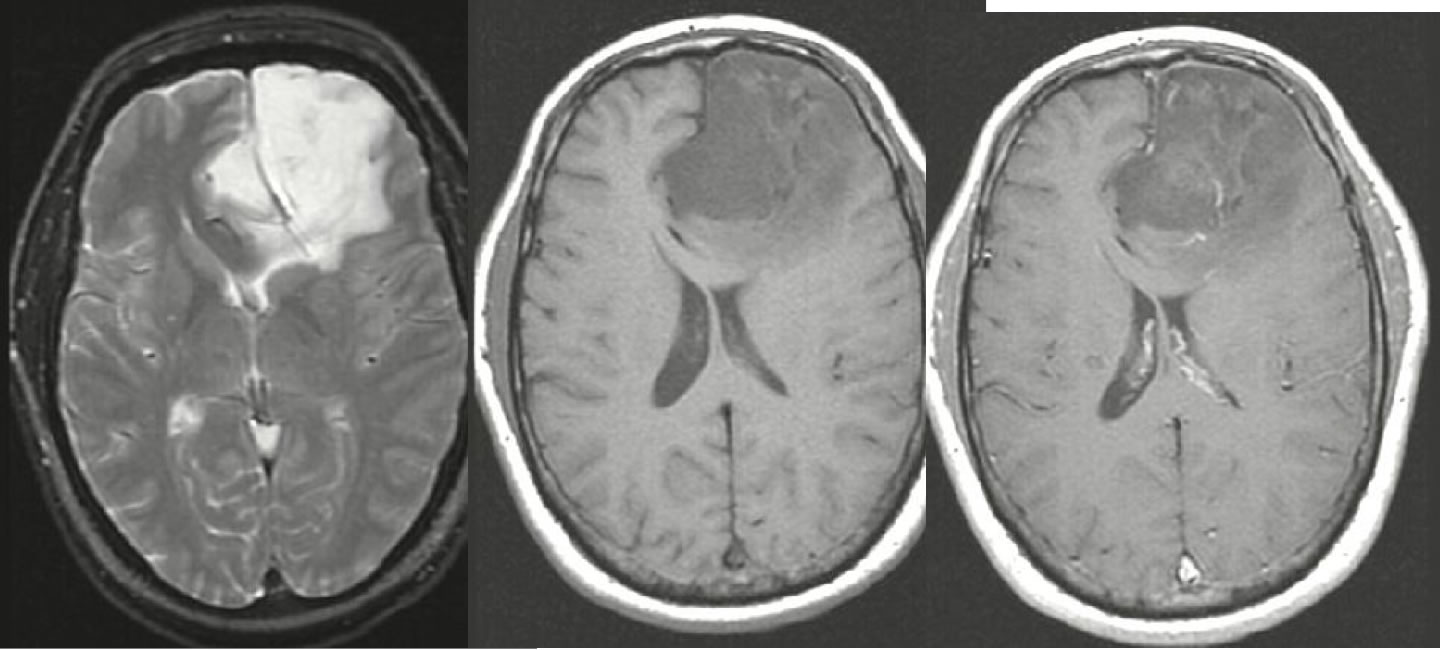
Oligodendroglioma
Findings:
Axial T2WI demonstrates a heterogenous hyperintense lesion in the left frontal lobe with extension into the right frontal lobe. The lesion appears hypointense on T1WI. There is local mass effect with compression of the anterior horns of the lateral ventricles and sulcal effacement.
Differential diagnosis:
Oligodendroglioma, astrocytoma, ganglioglioma, DNET, ischemia
Discussion:
Oligodendrogliomas are well-differentiated primary brain tumors that are slow growing but diffusely infiltrating despite a well circumscribed appearance. A long standing history of headaches and/or seizures is common. The majority of oligodendrogliomas are supratentorial, most commonly in the frontal lobes. Oligodendrogliomas may also involve the parietal, temporal, and occipital lobes, but infratentorial lesions are rare. Classic imaging findings show a mixed density hemispheric mass that extends to the cortex with calcifcations in 70-90% on CT. Oligodendrogliomas are the most common intracranial tumor to calcify. MR will show a heterogenous hypointense hemispheric mass on T1WI and a hyperintense mass on T2WI, with variable enhancement ranging from intense to none. Development of enhancement typically indicates dedifferentiation. Cystic degeneration may occur in up to 20% of lesions, but other findings such as hemorrhage and necrosis are rare. Due to the long standing nature of these lesions, calvarial remodeling/erosion may be present. Oligodendrogliomas occur with a peak incidence in the 4th and 5th decades of life with a slight male predominance. Local recurrence after resection is common, and malignant progression may occur, but CSF dissemination is uncommon. Median survival after diagnosis is 10 years. Most are WHO grade II lesions, with those demonstrating increased mitotic rate, neovascularity, and possibly necrosis considered anaplastic and WHO grade III. However, the distinction between grade II and grade III lesions can only be made histologically.
BACK TO
MAIN PAGE