Basilar Artery Thrombosis
Findings:
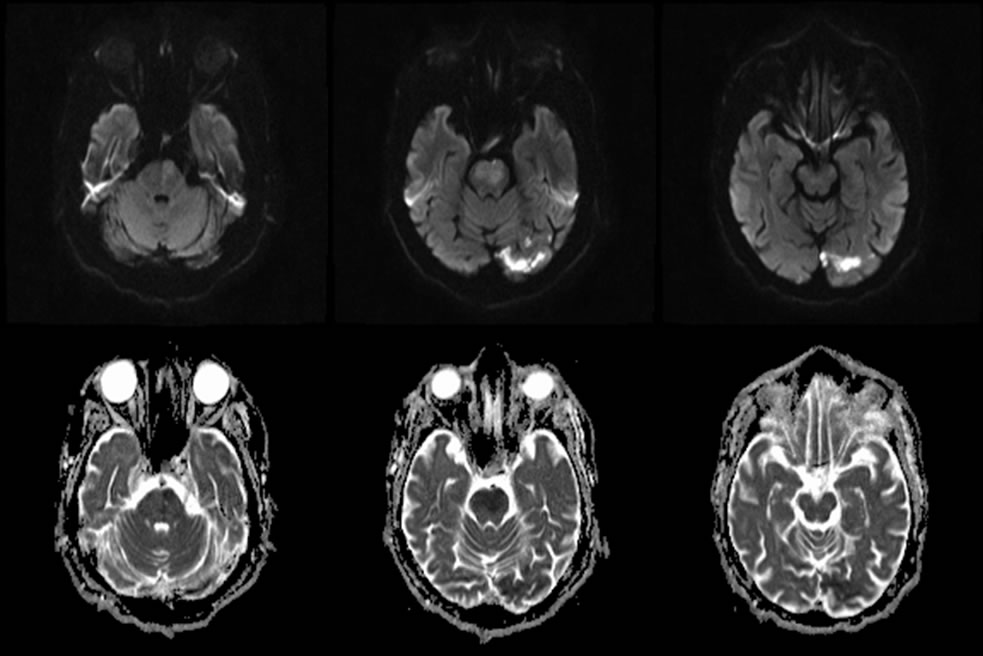
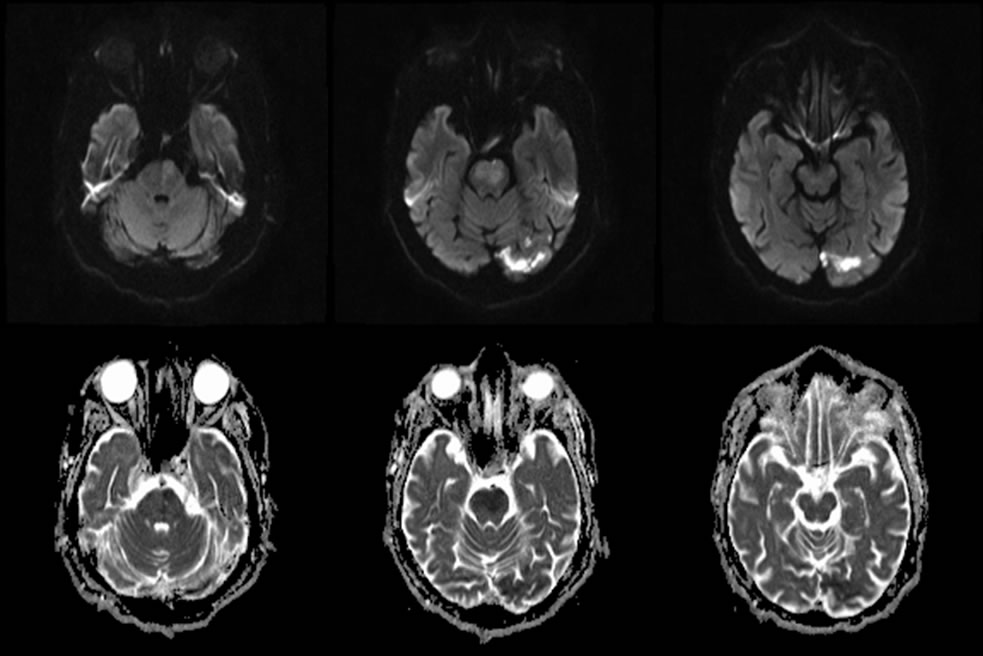
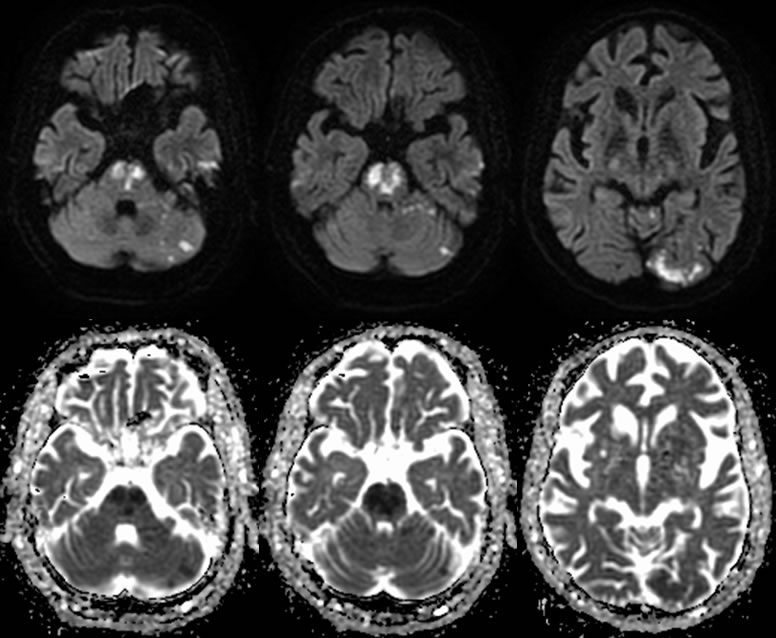
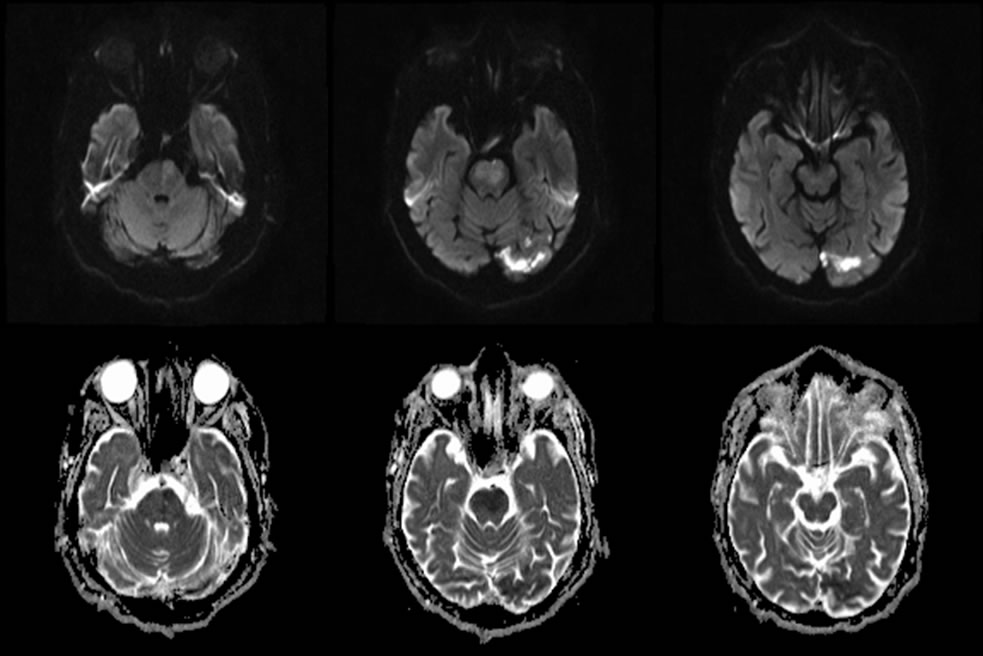
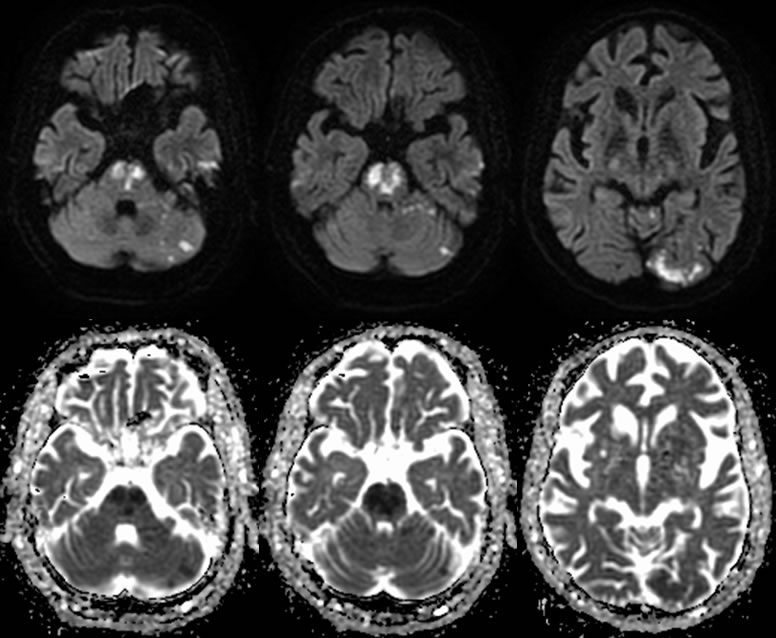
The two sets of axial MR images were taken at presentation and 48 hours later. They are included to demonstrate the evolution of stroke on diffusion weighted imaging (DWI) and apparent diffusion coefficient (ADC).
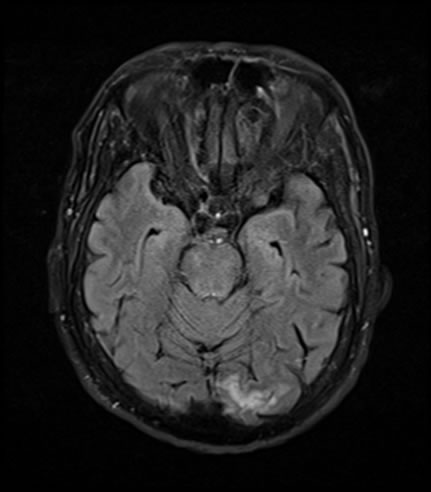
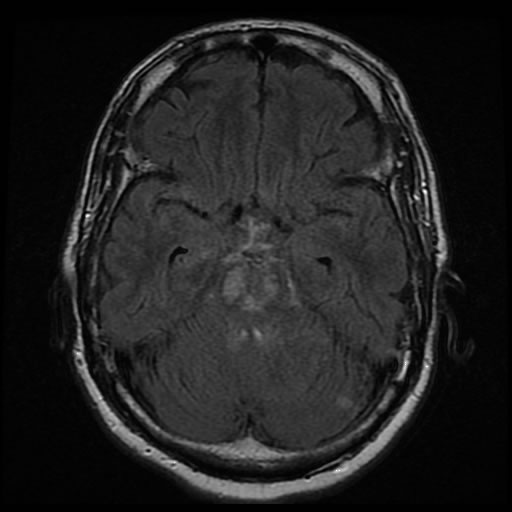
Axial DWI in the hyperacute phase demonstrates a patchy area of subtle hyperintensity within the pons. There is also an area of hyperintensity within the left occiptal lobe. These areas are hypointense on ADC. The pontine diffusion abnormality is not correlated with FLAIR hyperintensity initially, indicating hyperacute infarction.
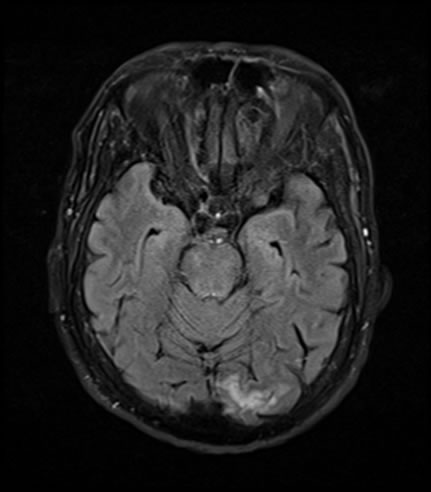
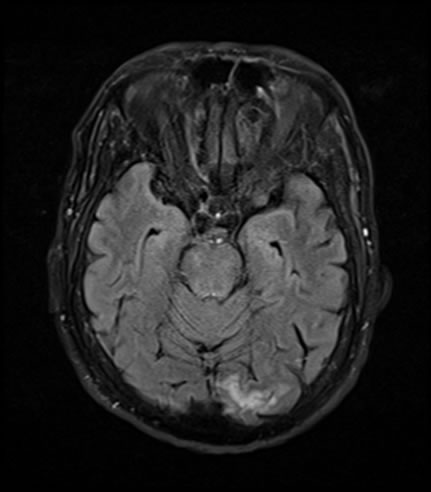
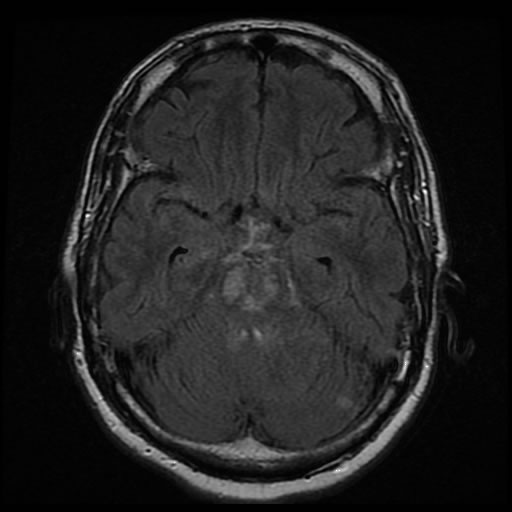
The MR imaging at 48 hours demonstrates that the previous area of subtle hyperintensity is now brightly hyperintense and has enlarged, representing progression and evolution of the infarct. There are also multiple new foci of restricted diffusion that have developed in the cerebellum and occipital lobes that are consistent with new posterior circulation infarcts related to basilar artery occlusion. Noted areas of infarct on DWI continue to be hypointense on ADC. FLAIR hyperintensity is now evident within the pontine infarction compatible with evolving cytotoxic edema.
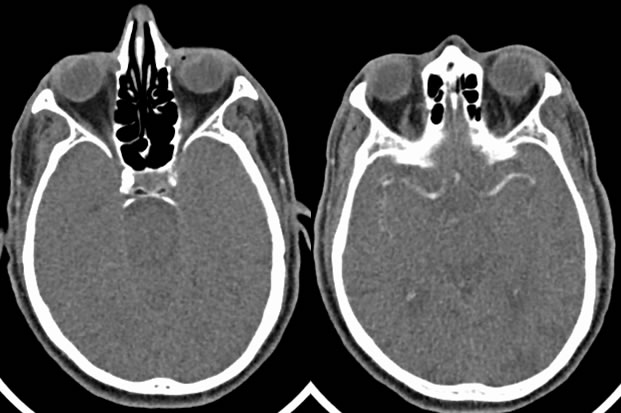
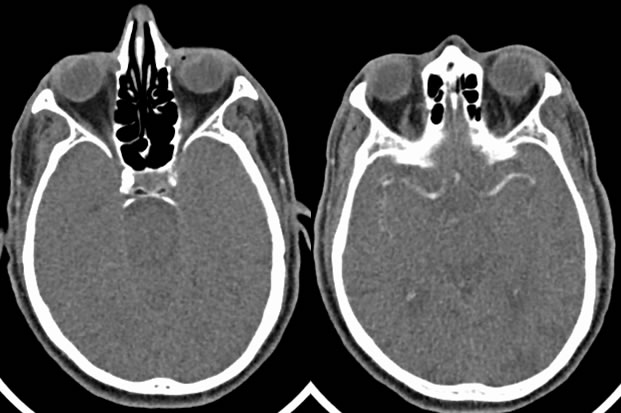
Axial CTA image demonstrates no contrast in the expected area of the basilar artery.
Discussion:
The basilar artery is the major blood supply of the posterior circulation of the brain and brainstem. As such, thrombosis in this vessel can be devastating. Up to 50% of patients may have nonspecific signs over several days that signal significant occlusion is imminent. These symptoms include headaches, visual disturbances, speech impairment, nausea/vomiting, dysarthria, and motor deficits. As in this patient, it is possible to have multiple infarcts in the posterior circulation distribution from small emboli breaking from the basilar thrombosis and may cause variable symptoms as well..With full occlusion of the basilar artery, it is possible that the patient may develop locked-in syndrome. This is due to ischemia of the ventral pons, which houses the corticospinal tracts, facial nerve nuclei, and lower cranial nerves. Locked-in syndrome, therefore, consists of full paralysis with relative sparing of eye movement and unaffected higher cortical function. Basilar artery thrombosis has high mortality, up to 90%, and high morbidity in survivors. Agressive treatment is warranted and is achieved through recanalization of the vessel.This typically consists of intra-arterial thrombolysis or mechanical embolectomy.
MR imaging of stroke is variable depending on the time since infarction. In the hyperacute setting (< 1 hour), there may be only subtle hyperintensity on DWI and hypointensity on ADC. The acute setting (0-7 days) is characterized by progressive hyperintensity over the infarcted area on DWI with a peak hypointensity on ADC happening around day 4. As the infarct ages during the subacute phase (1-3 weeks), the ADC will pseudonormalize then slowly become hyperintense. The DWI remains hyperintense during this period due to T2 shine through. After around three weeks the infarct is considered to be in the chronic stage, which shows continued hyperintensity on ADC and low signal on DWI and T2 shine through resolves.
Case contributed by Christopher Heald, UC M4
BACK TO
MAIN PAGE