Idiopathic Hypertrophic Pachymeningitis
Findings:
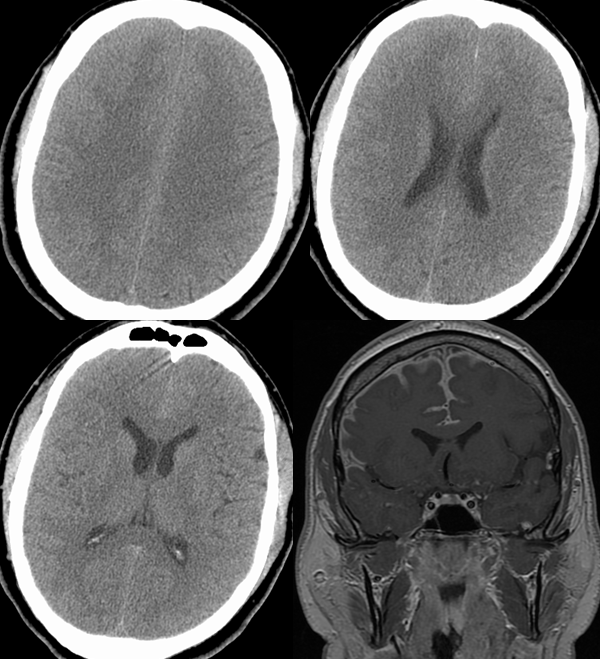
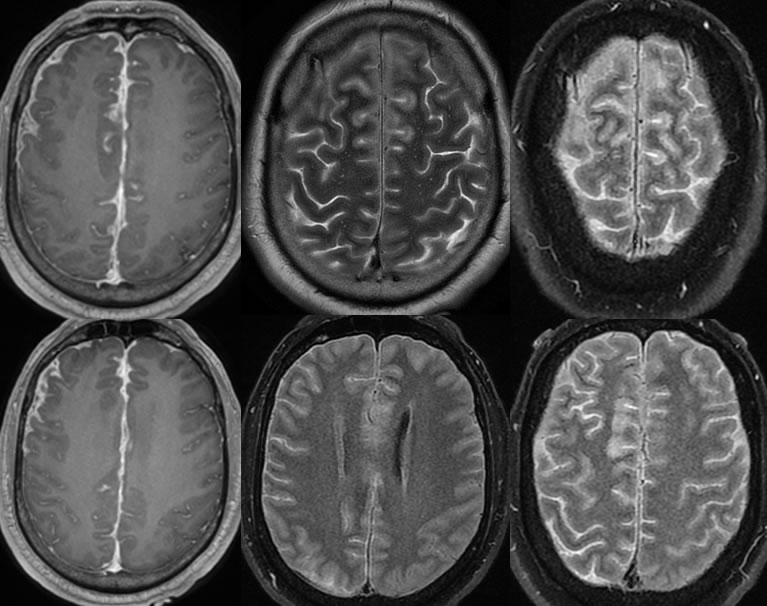
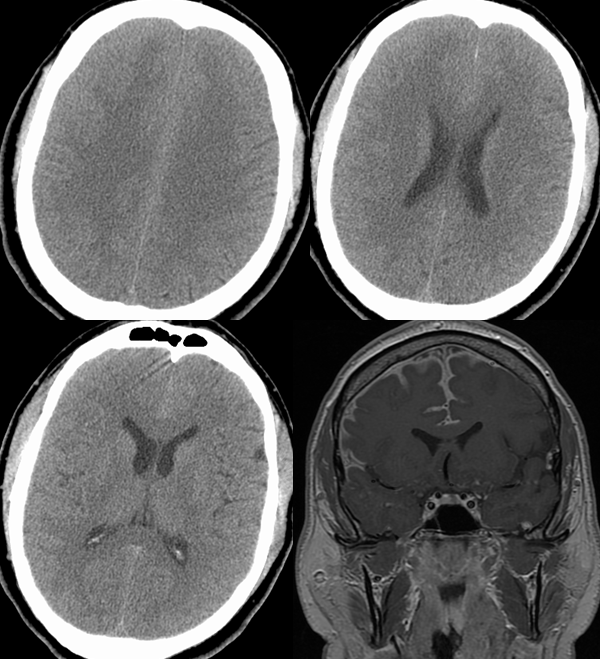
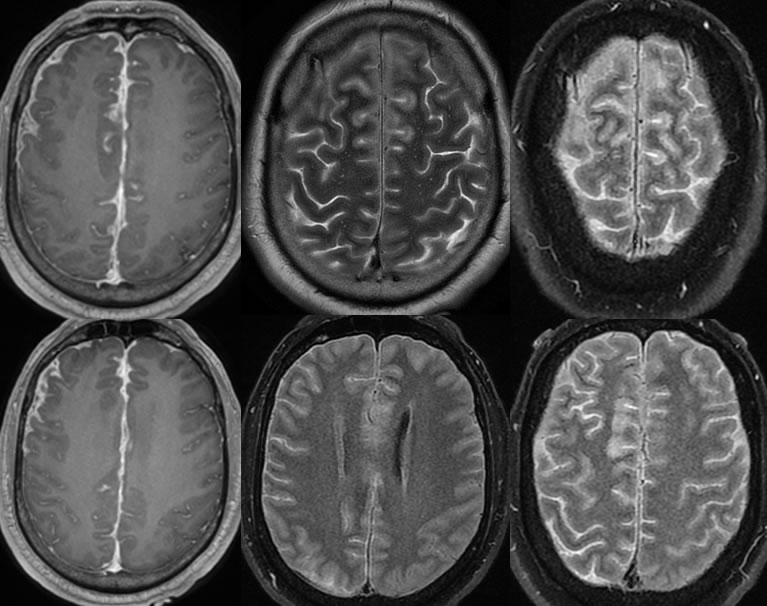
There is moderate enhancement in the right-sided hemisphere / convexities and to a lesser degree into the left convexity with probable associated dural thickening/enhancement in the right convexity and interhemispheric fissure/falx. There are also associated diffuse areas of hyperintense FLAIR signal in the bilateral sulci, right greater than left. Superimposed cortical T2 hyperintensities are present. On CT, the dural and leptomeningeal disease is relatively hyperdense to CSF causing obliteration of sulci particularly in the parasagittal regions.
Discussion/Differential Diagnosis:
DDx: Inflammatory (meningitis, sarcoidosis, rheumatoid, idioopathic, TB less likely), metastatic disease. Sequelae of remote subdural hemorrhage could have been considered if less and more uniform asymmetric dural thickening. Findings of low CSF pressure should be symmetric and will not include leptomeningeal enhancement.
This patient has a history of rheumatoid arthritis, therefore this is technically not idiopathic. Biopsy results were nonspecific chronic inflammatory. Localized inflammatory thickening of the dura can arise from a number of different causes including bacterial meningitis, rheumatoid arthritis, and neurosarcoidosis. Tuberculosis, syphilis, and Wegener's Granulomatosis may appear similar. Metastases or lymphoma may be indistinguishable by imaging. Clinical presentation will vary with the underlying cause but cranial nerve palsy including vision loss may be seen, and most will have headaches.
MRI will show localized or less commonly diffuse dural thickening. On T1 imaging with contrast, dural enhancement will be present, and T2 imaging will often show hypointense thickened dura compared to brain parenchyma. Occasionally, more focal masslike or plaquelike areas may simulate meningioma, termed tumefactive hypertrophic pachymeningitis.
The process typically will be progressive if left untreated, with progressive symptoms, but most patients have significant improvement with steroid therapy. Methotrexate and/or azathoiprine may be added in refractory/recurrent cases to decrease steroid load.
This case was prepared with the assistance of Joshua Hall, UC undergraduate
BACK TO
MAIN PAGE