 <
<
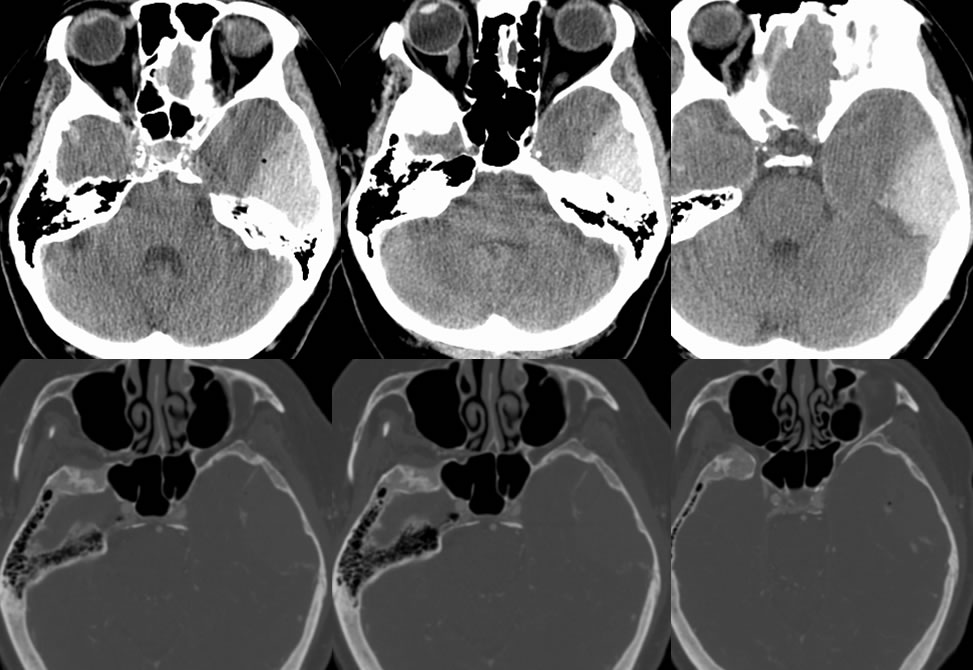
Epidural Hematoma with Active Extravasation
Findings:
A large left middle cranial fossa epidural hematoma underlies a subtle nondisplaced left temporal bone fracture. Linear hyperdensities along the periphery of the hematoma indicate active contrast extravasation from the left middle meningeal artery. There is also a tiny focus of pneumocephalus in this region.
Differential Diagnosis:
With a recent history of trauma, hemorrhage should be considered first for this appearance. A hyperdense extraaxial mass of other cause such as meningioma, dural metastasis, or extramedullary hematopoeisis could have a similar appearance on postcontrast study if there were no history of trauma.
Discussion:
An epidural hematoma (EDH) has a biconvex hyperdense noncontrast CT appearance and usually does not cross sutures unless diastatic, to distinguish from subdural hematoma. They tend to form rapidly and reach final size quickly, but up to 25% may show delayed development or enlargement. Heterogeneous swirling density may be seen with hyperacute lesions before coagulation. Chronic EDH will show peripheral enhancement. EDH are usually (90%) arterial in origin caused by fracture through the groove for the middle meningeal artery, but may also be venous (10%) when associated with other fractures near dural sinuses, and are easy to miss near the vertex. They are usually caused by trauma and are seen in up to 15% of fatal head injuries, but nontraumatic causes may uncommonly be seen such as coagulopathy, tumors and vascular malformations. Clinically, a lucid interval is seen in up to 50% after the trauma after brief loss of consciousness, then there is deterioration (sz, N/V, aphasia, coma). They are most common in males 20-40 years old, and are managed surgically with an overall 5% mortality rate. Bilateral EDH and posterior fossa EDH have higher mortality up to 25%.
This case was prepared with the assistance of Joshua Hall, UC undergraduate