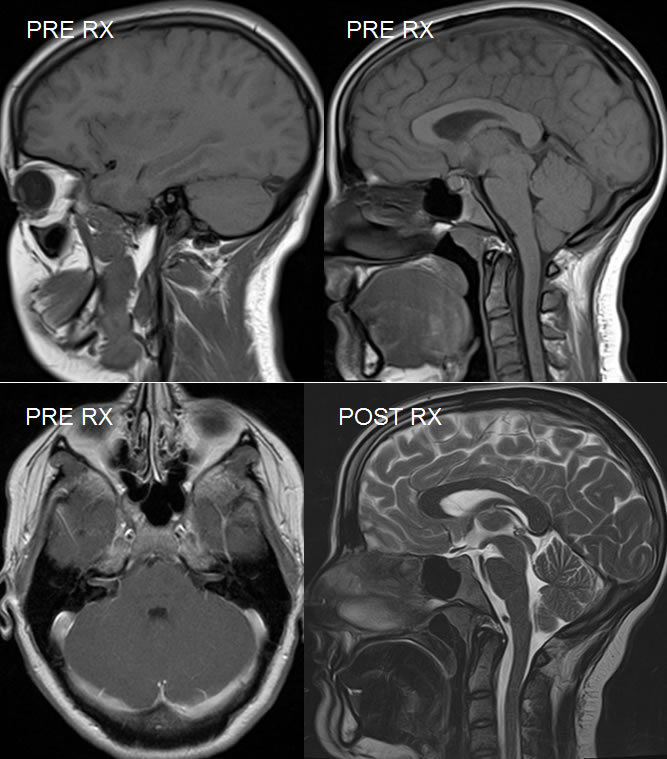
Intracranial Hypotension, resolved after blood patch procedure
Findings:
Sagittal T-1 weighted images demonstrate abnormal inferior displacement of the brainstem with interior descent of the cerebellar tonsils. The transverse sinus has an abnormal rounded cross section. The pituitary gland is prominent and there is horizontal orientation of the optic chiasm. Dural congestion is seen along the and upper cervical spine. The mammillary bodies are displaced well below the incisural plane. There is triangular pontine deformity and partial closure of the interpeduncular cistern.
Axial post contrast T1 weighted image demonstrates abnormal symmetric linear enhancement within both internal auditory canals. The dural sinuses are again noted to be engorged.
The post treatment sagittal T2 weighted image demonstrates normal findings. The brainstem and cerebellum tonsils have returned to normal position and the pituitary gland is no longer prominent. No significant residual dural congestion is seen. Normal height of the interpeduncular cistern is restored. The triangular pontine deformity has resolved.
Discussion/Differential Diagnosis:
Differential Diagnosis: Intracranial hypotension, Chiari I malformation
Abnormalities of CSF pressure, either low or high, are being increasingly recognized as potentially treatable causes of chronic headaches. While the classic low pressure headache is orthostatic, other types of headaches may occur including constant severe headache, pulsatile headache, and nuchal rigidity. Less commonly, cranial nerve palsies, visual disturbances, encephalopathy, coma, and death may occur due to advanced herniation. Symmetric smooth dural enhancement is the classic imaging finding seen in spontaneous intracranial hypotension (SIH), but its absence does not exclude the diagnosis.
Careful attention should be paid to the position of the brainstem on the sagittal midline image, particularly structures at or below the level of the incisural plane demarcated by a line drawn from the tuberculum sellae to the ICV confluence at the tentorial apex. The mammillary bodies should always be above this plane. Other findings that may be seen as a manifestation of brainstem sag include a horizontal optic chiasm, inferior bowing of the third ventricular floor, closure/effacement of the interpeduncular cistern, vertically oriented splenium, cerebellar tonsil extent to or below foramen magnum. The low CSF pressure tends to pull on the margins of the dura as a compensatory effect (Monro-Kellie doctrine- CSF and intracranial blood volumes vary inversely), therefore congestive changes of the dura, dural sinuses, and clival/epidural plexus may be seen along with subdural hematomas or hygromas, prominent pituitary, and a rounded rather than triangular cross sectional dimension of the dural sinuses. Extradural fluid collections may be seen particularly at C1-2, but do not necessarily indicate the site of leak.
Unfortunately, inferior cerebellar tonsillar descent is most easily recognized by the inexperienced viewer who is not familiar with the expected normal position of the brainstem and a diagnosis of ChiariI malformation is made, which then often condemns the patient to a needless suboccipital decompression procedure which will not cure the patient and usually makes things worse. Catastrophic herniation may occur. SIH is probably more common than Chiari I. In addition, patients with spontaneous SDH with no trauma or other underlying reason should be evaluated carefully for SIH because draining the SDH may make symptoms worse.
SIH can be caused by any factor leading to low CSF pressure, including a CSF leak from a dural tear (probably more common than previously thought) from even trivial trauma (vigorous coughing, minor fall, vigorous exercise), LP, overshunting, or ruptured diverticulum. Dehydration may contribute. Small dural tears adjacent to disc herniationsand osteophytes are reportedly rare but are likely more common that previously recognized. Up to 2/3 of pts with SIH have stigmata of a connective tissue disease (Marfans, ED) with expected weakened dura.
The treatment of SIH without an indwelling shunt is minimally invasive, with a nontargeted epidural blood patch initially performed, which may improve symptoms in 60%, with another 20% improving after the second blood patch. CT myelogram may be useful to determine the exact site of CSF leak which would allow for a targeted blood patch, with surgical repair of a dural tear rarely necessary. At the time of myelography, opening pressure can be checked which may be 6 cm H2O with SIH, and injection of intrathecal saline may acutely improve symptoms. After successful closure of the leak, the imaging findings return to normal with normal position of the brainstem restored, as above. Some patients successfully treated for SIH will then develop intracranial hypertension which is another topic.
BACK TO
MAIN PAGE