Dural Sinus Thrombosis with hemorrhagic venous infarcts.
Findings:
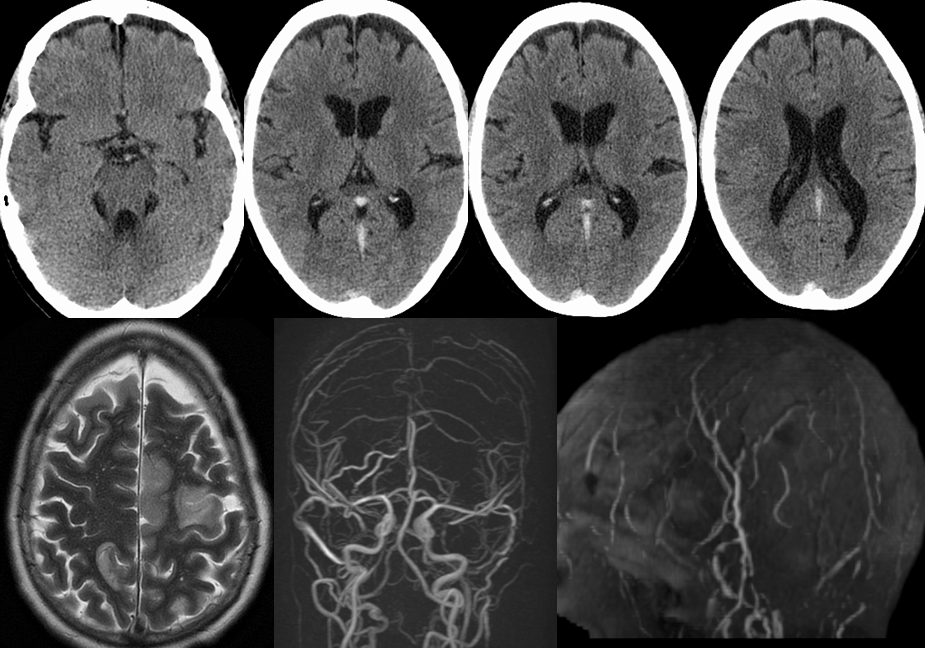
Axial noncontrast CT images demonstrate abnormal hyperdensity of the posterior margin superior sagittal sinus, straight sinus, and vein of Galen.
A single axial T2 weighted image demonstrates abnormal cortical hyperintensity within the left frontal parasagittal and lateral region as well as the right frontal parietal parasagittal region.
Reformatted MRV images of the head demonstrate absence of flow signal within virtually all intracranial venous structures.
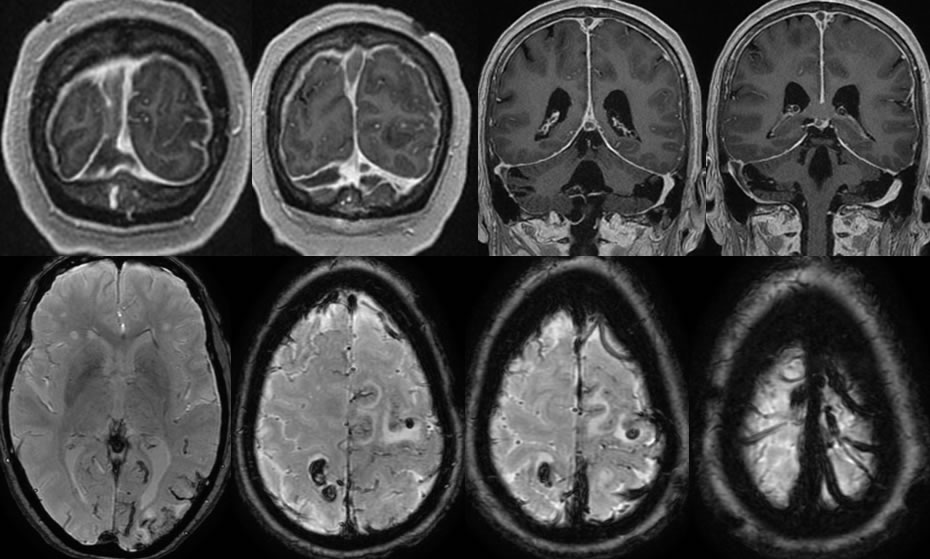
Coronal T1 post contrast images demonstrate large filling defects within the superior sagittal sinus, right transverse/sigmoid sinus, and the vein of Galen. There is diffuse dural enhancement and congestion.
Axial SWI images demonstrate abnormal blooming of the dural sinuses and cortical veins. Hemorrhagic foci are also present within the zones of T2 signal abnormality.
Discussion:
Dural sinus thrombosis (DST) is a uncommon etiology of stroke like symptoms (1%) and may present with headaches, nausea, and vomiting. Symptoms may range from asymptomatic to coma and death, and up to 50% will develop venous infarcts. DST is slightly more common in females and has a wide array (>100) of potential causes including coagulation disorders (protein C, S, PT mutations), dehydration/metabolic, OCPs, infection, trauma, and collagen vascular diseases among many others. While the above case is quite obvious, the imaging diagnosis may be difficult and many pitfalls exist. Noncontrast CT may show asymmetric hyperdensity of the dural sinus compared to arterial structures (pitfalls- hemoconcentration- look for asymmetric hyperdensity). A nonenhancing dural sinus filling defect (empty delta) is seen on MR and CE CT, with blooming of thrombus on GRE/SWI (deoxyhemoglobin). Other potential pitfalls include prominent arachnoid granulations (round, CSF signal), complex signal of variable flow and differing ages of blood products that may either simulate flow or thrombus, atretic/hypoplastic sinus w or wo gaps (R tx sinus dominant >50%, L dominant 25%), and foci of fat. Venous infarcts can show enhancement that mimics neoplasm. Chronic DST can enhance and simulate flow, but signal on other sequences will likely be abnormal. The parenchymal signal abnormalities are more likely to be reversible than those related to arterial occlusion. DST is treated with anticoagulation with consideration for endovascular therapy if extensive.
Please refer to these cases for additional examples and discussion of dural sinus thrombosis:
-Superior sagittal
sinus thrombosis
-Superior sagittal
sinus thrombosis2
-Straight sinus
thrombosiS
This case was prepared with the assistance of Joshua Hall, UC undergraduate